
Linda Mama
Following a Government directive in June 2013, maternal health services would be free in all public health facilities. Provision of high quality maternal delivery services in public health facilities has been a key focus of UHC under the Big Four Agenda, alongside the Managed Equipment Scheme (MES), to lower maternal, infant and neonatal mortalities and ensure every child gets the recommended vaccines.
The Free Maternity Services programme was rolled out in all public health facilities in 2013 to eliminate financial barriers and high cost of treatment in accessing maternity services at public hospitals, and to address geographical and infrastructural challenges that hinder access to the services and social-cultural barriers.
This resulted in an increase in the number of skilled deliveries from 600,323 to 950,000 annually. Since the introduction of free maternity services on 1st June, 2013, deliveries under skilled attendants significantly increased from 44 percent to 62 percent in 2016/17, with a drop to 57 percent in 2017/18 due to health workers strikes/unrests that were experienced throughout the country; this is a significant increase of over 360,000 skilled deliveries between 2013/14 and 2017/2018.
As part of the movement towards UHC, the Government has expanded social health protection by implementing the Linda Mama, Boresha Maisha programme targeting mothers and their infants.
Late referral to health facilities, health worker strikes, and quality of care including inadequate staff and medical equipment, remain the main issues in the number of maternal deaths.
The main objectives of the programme are;
- To promote and encourage women to give birth in health facilities, and therefore contribute to improvement of pregnancy outcomes, including maternal and neonatal deaths;
- To secure household incomes meant for maternity facilities to other economic activities with a potential positive impact on poor households;
- To supplement the public health budgetary requirement to effectively address access and quality gaps to improve service delivery;
The Ministry allocated a budget of Ksh4.298 billion in FY 2017/18 to ensure that all facilities were reimbursed for their health services. The National Health Insurance Fund (NHIF) received premiums for the programme amounting to Ksh3,361,525,853 in the financial year 2017/2018.
This programme has seen the number of deliveries at public health facilities in the country increase from 925,674 (2014/15), to 995,946 (2015/16), and drop to 962,885 (2017/18). A total of Ksh12.2 billion has been transferred to public health facilities offering the free service.
This has also necessitated a change in the way the programme is implemented to ensure increased coverage and benefits to mothers. From the final quarter of the 2016/17 financial year, the programme was implemented through the NHIF, covering antenatal care, deliveries, postnatal care and other newborn illnesses..
The service was also available all over the country in both public and private not-for-profit healthcare providers interested in joining the programme.
The total number of beneficiaries for the FY 2016/17 was 987,122 against an expenditure of Ksh3.54 billion, while for Linda Mama, 762,661 expectant mothers have been registered and a total of Ksh1,487,620,052 has been paid out for 516,906 deliveries, covering both inpatient and outpatient care.
A total of 209,637 ante-natal care and 35,245 post-natal care visits have been recorded.
The Health Act of 2017 is also paving the way for the implementation and development of other health-related legislative instruments that will address health rights as per the Constitution.
The ministries of Health and Agriculture, Livestock and Fisheries approved and signed the National Policy for the Prevention and Containment of Antimicrobial Resistance in Kenya ― and its national action plan on the prevention and containment of antimicrobial resistance ― in June 2017.

The Kenya Quality Model for Health (KQMH) has been reviewed and forms the basis for Quality of Care measurement and accreditation. Some 40 counties had their County Health Medical Teams (CHMTs) trained on Quality Improvement approaches as enshrined in the KQMH for equipping health professionals with skills and knowledge in Quality Improvement for improved delivery of health services.
Partners in Linda Mama include the African Health Markets for Equity (AHME), which is supported by the Bill and Melinda Gates Foundation, and the UK Department for International Development (DfID). The programme is supported to deliver health services in public and private health facilities in partnership with PharmAccess Foundation, Population Services International (PSI), and Marie Stopes International.
A case study of the Linda Mama programme by PSI and Marie Stopes for AHME made interesting observations that they shared with the Ministry of Health.
They noted that the Linda Mama programme is more attractive to health providers contracted by NHIF for its in-patient and out-patient services, but they are affected by inconsistent and unpredictable disbursement of funds.
Another interesting finding was that increased NHIF enrollment has changed the business strategies of healthcare providers, because it strengthened their social franchise value proposition.
The Linda Mama scheme was introduced in three phases:
- Phase 1, from April 2017, targeted faith-based facilities and the private sector;
- Phase 2, from July 2017, targeted the public sector;
- Phase 3, from March 2018, added antenatal care (ANC) and post-natal care (PNC) services to the benefits package.
The reimbursements rated are in tiers, determined by the level of care offered by the provider.
Tariffs for public health facilities are therefore lower, while private sector tariffs are slightly high.
The Linda Mama, Boresha Jamii programme being implemented by the Government through the NHIF, seeks to improve the efficiency and performance of the Government’s initiative on maternal and child healthcare.
NHIF was chosen because of its expanded provider network to public, private and faith-based health facilities, and its mobile registration platform to track beneficiaries of the cover. Under it, women get access to a one-year expanded package of benefits consisting of antenatal and postnatal care, deliveries and care for the newborn.
The focus is on equity, access, affordability and quality. Under the Linda Mama, Boresha Jamii programme, public health facilities that provide maternity services are assured of funds to supplement their regular budgetary allocations to address gaps in provision of services.
Since its implementation, the number of deliveries in public health facilities has continued to grow.
By enrolling private health facilities and providers in the Linda Mama programme, NHIF is championing UHC by increasing access to quality primary health services for the poor in difficult-to-access areas.
The NHIF is also considering a number of options to increase participation of the private sector in the Linda Mama programme. They include:
- Introducing a standardised reimbursement rate for normal deliveries in private healthcare facilities to ensure quality at all levels of care.
- Insisting on a standardised contract for all private healthcare providers to eliminate delays in claims processing and reimbursements caused by variations in contracts.
- Working with county departments of health to increase public awareness of the scheme, and boost participation by poor and marginalised women, who are the main targets.
A key indicator that Linda Mama is impacting positively on UHC can be seen in the increase in pentavalent third dose immunisation countrywide.
This type of immunisation is used as a global measure of the number of children who have received the full regimen of immunisation. There was an increase in pentavalent vaccine uptake by 18.1 per cent from 1,064,500 in 2017 to 1,299,700 thousand in 2018.
Immunisation coverage for infants increased from 68.4 per cent in 2017 to 81.6 percent in 2018. The decline in the number of infants vaccinated in 2017 is attributed to industrial action by health workers.
Access to safe blood transfusion
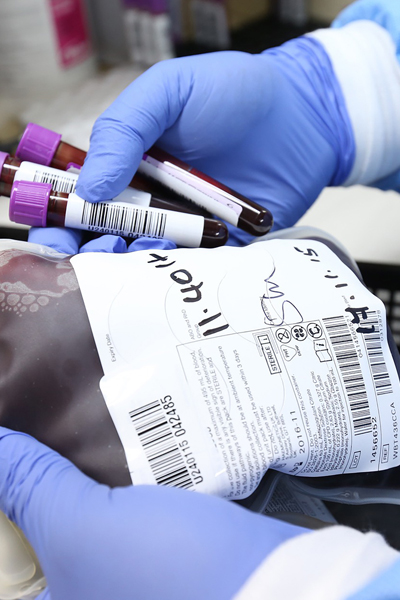 A key goal of Kenya’s UHC is access to safe blood transfusions. This includes providing access to up-to-date information and strategies on blood safety and access, and a sustainable national blood programme all the way from planning and implementation to monitoring.
A key goal of Kenya’s UHC is access to safe blood transfusions. This includes providing access to up-to-date information and strategies on blood safety and access, and a sustainable national blood programme all the way from planning and implementation to monitoring.
From 1985, with the advent of HIV/Aids, reduced blood collections, increased cost of blood, and higher emphasis on blood safety, became more critical.
In 1994, Kenya recognised the need to set up a national blood service in line with WHO recommendations. Recommendations were made to establish a regional network of transfusion centres under central coordination.
In 2001, Kenya’s first-ever blood policy guidelines were developed and launched and the first regional blood transfusion centre (RBTC) and national coordinating office were established in Nairobi.
Progressively, six regional and nine satellite centres have been established and blood policy guidelines and national standards developed. There is also increased hemovigilance ― the set of surveillance procedures covering the entire blood transfusion chain, from the donation and processing of blood and its components, through to their provision and transfusion to patients, and including follow-up.
Key to all these is the setting up of RBTCs in Nairobi, Nakuru, Mombasa and Embu. Today, 100 percent of collected blood is screened for HIV, HBV, HCV and syphilis.
There has also been a massive improvement in donor selection and deferrals, resulting in lower sero-prevalence. The Kenya National Blood Transfusion Service (KNBTS) has adopted the appropriate blood testing algorithm in line with WHO recommendations.
Each centre is equipped with a cold room for storage and appropriate blood bank fridges with a capacity of up to 5,000 units of blood. Unsafe units are sorted and incinerated.
Also, each centre has an incinerator and standby generator, while safe units are stored at appropriate temperatures. RBTCs maintain proper blood inventory by type and product, and blood is released to the user institutions as per their orders, subject to availability of stock.
KNBTS supplies blood and blood products to both public and private hospitals and ensures that there is a cold chain up to the hospitals. Blood use guidelines have been developed and distributed by KNBTS and quality is assured via HIV testing and counselling centres (HTCs) linked to hospital transfusion units.
Monitoring of blood use, haemovigilance and investigations of adverse transfusion reactions are also done through HTCs.
The Government has recognised the need for KNBTS operations to be self-sustainable to avoid a lapse when donor funds trickle out. Among the measures taken is increased funding to KNBTS and provision of adequate blood storage facilities at the hospitals.
Lack of a legal framework has been addressed via the Health Act of 2017, allowing for mobilisation of support at national, regional and global level. This allows foreign governments and development partners to invest in, strengthen and sustain national blood programmes.
An additional strategy is public education to raise awareness on the need for voluntary blood donation, patients’ rights, and informed consent as a foundation for universal access to safe blood transfusion.
International best practice, the WHO , and Kenya Blood Policy, recommends that patients should be transfused with the component of blood they require as opposed to giving them whole blood.
It has also been shown that close to 95 percent of all transfusions require blood components and only about five percent require whole blood. Also, one third of all transfusions go to children who require smaller blood volumes compared to adults.
To comply with best practice, KNBTS converts a certain percentage of the whole blood units collected into various blood components ― namely packed red cells, platelets, fresh frozen plasma and cryoprecipitate.
It also prepares small packs for children. This process requires dedicated skilled staff, special blood bags, and appropriate infrastructure including transport and blood storage equipment. Kenya has approximately 561 transfusing facilities (government, faith-based and private) which get blood from KNBTS. However, KNBTS is only able to meet 52 percent of their total needs.
In three years, a total of 158,749 (2015-16), through to 158,378 (2016-17) and to 160,000 (2017-18) blood units were collected. This is about 38 percent of the national demand for blood. The shortage led to many preventable deaths of mothers and children.
In 2015, Kenya became the first country in East Africa to fully automate it blood bank processes when the KNBTS installed an electronic system in its national office and all the RBTCs, covering the entire country.
The ePROGESA software solution was specifically designed to meet the functional requirements of blood banks and blood transfusion centers. It enables the blood bank to keep track of donors and units of blood available in all its facilities, which ensures the traceability of blood and blood products from collection to distribution.
The system also enables an interface of the various processes to ensure quality and safety measures are enforced, right from collection to administration of the blood to needy patients.
Global Communities supported the installation and training of KNBTS staff on management of the software under the Kenya Blood Safety Programme (BSP). The five-year programme, funded by the US Center for Disease Control and Prevention (CDC), was instrumental in strengthening the capacity of KNBTS to ensure a safe and sufficient blood supply in Kenya.
The programme’s key contributions include developing guidelines on the establishment of blood transfusion facilities. The BSP also helped to increase blood collection and testing levels. As a result, the KNBTS is now collecting more blood than before.
Additionally, the programme supported KNBTS to become more transparent in its planning and budgetary processes, helping it develop an asset registry and set goals. The BSP also mapped all of the transfusing hospitals in the country on an interactive map so that KNBTS can better organise their service and plan for new facility sites; trained engineers on how to repair and maintain the specialised equipment; and advised KNBTS on how to improve service during blood donations.
The private sector is also supporting the Government’s efforts to increase supply of blood to hospitals.
Amref Health Africa and technology solutions firm Advanced IT Solutions (AISL) have partnered to boost blood supply using a Blood Services Information Management System known as Damu – Sasa.
The solution is an innovation borne of the Presidential Digital Talent Programme (PDTP) launched by President Uhuru Kenyatta in 2015.
Damu – Sasa was developed to maintain up-to-date information in the blood services value chain. This includes maintaining an accurate donor databank through which timely appeals for donations can be made during emergencies, ensuring real-time observation of blood level fluctuations and improving their real-time reporting.
In addition, through information sharing, Damu – Sasa enables collaboration among players in the blood services ecosystem, thus making blood services management more efficient and effective.
Through this partnership, Amref Health Africa provides support to AISL by marketing the technology solution, developing health-related content, promoting associated advocacy and offering other technical support. AISL, in turn, will focus on rolling out the Damu – Sasa solution, supporting clients and enhancing solutions.
The innovation ensures that blood banks have accurate data to improve effective use of blood as well as help with targeted donor appeals.
Kenya Expanded Programme on Immunisation

The Ministry of Health established the Kenya Expanded Programme on Immunisation (KEPI) in 1980 with the aim of providing immunisation against the then six killer childhood diseases; namely tuberculosis, polio, diphtheria, whooping cough, tetanus and measles to all children in the country before their first birthday, and tetanus toxoid vaccination to all pregnant women.
KEPI was part of the global Expanded Programmes on Immunisation (EPIs), whose main goal was to control killer, vaccine-preventable diseases of childhood.
Prior to 1980, vaccination services had been provided on an ad-hoc basis, mainly through primary schools and larger health institutions and facilities. During the late 1970s the National Public Health Laboratories of the Ministry of Health (NPHLs) used to manufacture smallpox and cholera vaccines, besides investigating all outbreaks of public health importance in Kenya.
Because of their role in the surveillance for and response to diseases of public health importance, the NPHLs became the repository of all emergency vaccines such as cholera, Hepatitis B, typhoid, rabies and anti-snake venom.
However, with the global eradication of smallpox, the NPHLs ceased manufacturing the smallpox vaccine, but continued to coordinate the use of other emergency vaccines, except for cholera, which was phased out in the 1980s due to poor efficacy.
From the early 1970s when international regulations mandated that people moving across countries must be appropriately vaccinated to prevent global transmission of regional endemic diseases, the Nairobi City Council coordinated the vaccination of prospective overseas travellers with cholera and yellow fever vaccines.
Subsequently, this role was taken up by the Department of Environmental Health within the Ministry of Health and was administered through the Port Health Services in collaboration with the Department of Immigration.
The KEPI programme concentrated initially on establishing and strengthening health service delivery. However, in the 1990s, having achieved the Universal Child Immunisation goal of at least 80 percent of the target population, KEPI’s focus changed to disease control, elimination and eradication.
The immunisation programme is managed by the Unit of Vaccine and Immunisation Services (UVIS) within the Ministry of Health. The unit’s mandate is to coordinate vaccination services for all preventable diseases through the provision of guidelines, selected priority vaccines, and related biological sera such as immunoglobulins.
Apart from routine infant vaccines, the unit also provides vaccines for high risk groups (tetanus for special occupational risk groups, Hepatitis B vaccines for health workers, typhoid vaccine for food handlers, yellow fever vaccination for foreign travellers, emergency anti-rabies vaccine, snake anti-venoms and any other vaccines as may be prescribed during outbreaks).
The roles of the Unit of Vaccines and Immunisation Services (UVIS) are:
- Policy regulation and oversight;
- Commodity security and quality assurance;
- Monitoring and evaluation;
- Advocacy and resource mobilisation;
- Capacity strengthening; and,
- Conducting appropriate operational research.
The 47 county governments are responsible for health service delivery in their jurisdictions. The counties are responsible for hiring healthcare providers, training health service providers and management of cold chain equipment at the county, sub-county and facility level. They are also responsible for vaccine distribution and response to advance effects following immunisation (AEFIs) within the counties in collaboration with the national government and immunisation services.
UVIS is responsible for forecasting of vaccines, procurement, storage at the national and regional stores, and distribution from the airport to the regional stores.
The county governments are responsible for storage of vaccines in county stores, sub county stores and at facility level, and distribution of vaccines between these levels.
The Government of Kenya currently procures all traditional vaccines (measles, BCG, tetanus toxoid and polio vaccines), non-EPI vaccines such as Hepatitis B, typhoid vaccine and biological sera such as anti-snake venom and anti-rabies antibodies.
The Government also co-pays for Gavi-supported vaccines such as PCV, rotavirus, pentavalent and yellow fever. The procurement of vaccines is done through Unicef for traditional vaccines and for Gavi-supported vaccines, while the nonEPI vaccines are bought through public procurement procedures through the Kenya Medical Supplies Authority (KEMSA).
The County governments are also responsible for procurement of non-EPI vaccines and biological sera through KEMSA. Vaccine distribution and storage responsibilities are shared between the National and County governments. The National government is responsible for storage and distribution from the airport through to the national and regional vaccine stores.
The county governments are responsible for collecting vaccines from the regional stores, for distribution and storage of vaccines, and maintenance of cold chain equipment at the county, sub-county and facility levels.
The vaccine cold chain and repair system is a challenge and UVIS, together with strategic partners, is working to ensure that the Replacement, Expansion and Maintenance (REM) plan is implemented. The cold chain management system is also facing a challenge with the introduction of new technologies such as solar direct drive and continuous temperature monitoring systems, and the current gap in technicians’ skills and abilities is glaring.
When skills and abilities are available, there are challenges with resources to support installation, and repair and maintenance of equipment. Procuring spare parts and mobilizing staff is also a challenge.
Vaccine procurement has also faced several challenges with securing and ring fencing funds for vaccine procurement. This is due to devolution of funds that were secured in the previous system. The Ministry of Health is working to ensure that funding for vaccines and co-financed vaccines is ring fenced.
These challenges have been reflected by the defaulting on Gavi co-financed vaccines in the financial year 2013/2014. However, the Ministry of Health has made several improvements in improving vaccine procurement, vaccine supply, and the cold chain and logistics system.
The Ministry has outsourced the distribution of vaccines between the national and regional vaccine stores to several private sector companies that manage and distribute vaccines in refrigerated trucks. The outsourcing has successfully been managed by the Unit of Vaccines from 2013.
The outsourcing has improved the speed and efficiency of vaccine delivery, quantity of vaccines delivered, and improved the temperature maintained during transportation. The Unit of Vaccines has also developed an online reporting system for vaccines from the national to the regional vaccine level, and is implementing the same system at the sub-county stores.
The Unit of Vaccines is developing the system with support from the Clinton Health Access Initiative (CHAI), Unicef, USAID’s Maternal and Child Health Integrated Program (MCHIP) and the WHO. The system will also integrate with the national reporting system. The unit has also made changes to the temperature monitoring system to ensure that the vaccine cold chain is maintained at high quality through deployment of Fridge-Tag2, a continuous temperature monitoring device, in all health facilities – this has replaced the thermometer at all levels.
The unit is also working to introduce remote temperature monitoring devices in larger vaccine stores and cold rooms through the introduction of Remonsys temperature monitoring devices.
Vaccine service delivery is a function of the County governments. They are responsible for service delivery at facility level. The counties are also responsible for hiring, training and supervision of healthcare workers, and management of health facilities.
Following devolution of health services, the current roles for the National government are: policy direction, standards and quality assurance, capacity building, immunisation services monitoring, procurement of vaccines, limited logistics, resource mobilisation, and responding to outbreaks. County governments are mandated by the Constitution to manage health service delivery, mobilise resources, monitor delivery of services, and mobilise communities to demand and utilise services.
The National government’s responsibilities in service delivery are mainly to develop standards and training guidelines for the counties to implement.
The National government offers technical assistance by training the county health management teams, providing technical assistance, and ensuring that quality standards in service delivery are well known and adhered to.
The County Governments are responsible for generating information on immunisation services offered and reporting the information through DHIS-2, which is a management information system. The county is responsible for developing and analysing county level immunisation coverage and other related data.
The counties face several challenges in their ability to critically analyse the immunisation data reported and developed at the county, and in using the information to develop plans. The challenge in technical skills at the county level is also worsened by loss of healthcare workers due to movement from volatile counties and transfer of trained health workers within and between different counties.
As Kenya implements devolution, improving and sustaining national immunisation outcomes will be crucial.
Surveillance is a key component of immunisation services, which can be sub-divided into two:
- Surveillance activities that help the system to be sensitive in detecting and reporting on priority diseases;
- Surveillance of accelerated disease control, which includes vaccine preventable diseases like measles, polio, neonatal tetanus, maternal neonatal tetanus, rotavirus and meningitis.
Disease surveillance activities are implemented in the 47 counties, which comprise 292 sub-counties. Networking strategies between the National and County governments are in place to ensure that the gains are not lost, but sustained in a manner that will achieve the global polio eradication goals.
Kenya and other Horn of Africa countries remain at risk of imported wild poliovirus from neighbouring Somalia, as in the 2013 outbreak that continued until July 2014. In 2014, all the 47 counties reported Acute Flaccid Paralysis (AFP) cases, with 45 (97 percent) having a non-polio AFP detection rate greater than 2.0/100,000. AFP is the most common sign of acute polio.
All but four counties (Kericho, Marsabit, Busia and Muranga) had stool adequacy greater than 80 percent. To improve AFP surveillance, the Ministry of Health and key partners have rolled out community disease monitoring in Garissa, Wajir and Nairobi.
After the polio outbreak in May 2013, the country initiated environmental surveillance for polio viruses in an effort to supplement AFP surveillance, which is the gold standard for monitoring the wild polio virus.
Rotavirus surveillance was introduced at the Kenyatta National Hospital (KNH) in 2006. It documented the burden of rotavirus disease, and thus formed the baseline information for the introduction of the rotavirus vaccine in Kenya. Further, sentinel surveillance continues at the sites so as to inform on the effects of the vaccine after its introduction in July 2014.
The Disease Surveillance and Outbreak Response Unit (DSRU) has also continued to facilitate activities towards containment of the laboratory wild polio virus and has developed activities towards this end, following the establishment of an effective surveillance system for wild poliovirus eradication.

Further, the DSRU gets weekly reports from all sub-counties through the Integrated Disease Surveillance and Response (eIDSR) web-based system. However, the District Health Information System (DHIS) is more comprehensive.
Surveillance activities done in the past included capacity building of health workers on vaccine preventable diseases (VPD), IDSR and laboratory surveillance, which helped achieve the objective of strengthening and sustaining reporting of priority diseases, and the active case search for VPDs. However, high staff turnover due to devolution, among other reasons, has left many counties with staff who are not trained in disease surveillance, and more specifically VPDs.
There is low government funding for immunisation operations. Therefore, there is a need to increase funds allocated for operations from Ksh3.3 million to KshSh100 million by 2018, to determine allocations at county level, and increase the allocations.
The Ministry of Health has been facing challenges in timely disbursement of funds to Gavi before December 15 every year. This has been due to challenges in mobilising funds from the National Treasury in a timely manner.
Devolution of health services, including immunisation, has provided opportunities to increase access. More health facilities are being built in regions that suffered years of marginalisation. The devolved structures also provide opportunities to further disaggregate data for action.
Challenges during the past two years include underfunding, low prioritisation of immunisation, delivery, weak coordination of programmes and delayed procurement and related logistics, leading to stockouts.
New healthcare providers have been employed and managers appointed to provide immunisation services. This has created a pool of vaccinators and EPI managers who do not possess the prerequisite knowledge, skills and competencies to improve service delivery. The northern counties in Kenya continue to suffer insecurity that has affected delivery of quality services.
Due to insecurity and high population movement in the Horn of Africa (HoA) there is continued risk of VPDs.
The multiyear plan identifies the following key strategies: Advocacy with key decision makers and stakeholders at National and County governments to prioritise investing in immunisation services, improving linkages with communities and other health programmes, including reproductive, maternal, newborn and child health (RMNCH), HIV/TB/Malaria, and civil registration (CRD), with the county administration playing a key role in mobilising additional resources for immunisation services.
Use of quality disaggregated data to address inequities in access and utilisation of immunisation services by the poor and less educated remains key to reaching the 20 percent of children that have been consistently missed for the past three years.
Use of new technologies for knowledge management, and exchanges and linkages with professional accreditation systems are the innovative approaches identified to address the knowledge and skills gap among healthcare providers. PIRI has specifically been identified as a key strategy to ensuring delivery of services to insecure regions.
The following are key gains:
- Disease surveillance reporting structures are now in place;
- There is availability of standardised reporting tools at all levels;
- Devolution has decentralised many services but counties must prioritise surveillance operations;
- There is a good laboratory network for confirmation of cases;
- There is an active logistics management team at national programme level;
- There is ample cold storage capacity at national and regional stores;
- A clear logistical pipeline/structure exists at all levels;
- There is a reliable vaccine inventory management tool;
- EPI now has focal points in every county;
- Cold chain technicians are available at national and subnational levels;
- A waste management policy exists at national level, and is implemented in partner-supported areas;
- DHIS is regularly providing data on vaccine consumption;
- There is high community acceptance of immunisation;
- Communities across the country are generally more aware of the importance of immunisation;
- Healthcare workers are more knowledgeable on the importance of immunisation.
Disease surveillance and response used to be part of the larger EPI programme. A separate unit was created for ease of management and disease surveillance and response. After devolution, most staff in the counties had limited knowledge and huge training gaps. These are now being addressed.
Laboratory support services are being revamped to handle the increasing number of test samples from the field. Action is also being taken to address adverse events following immunisation (AEFI), which were initially poorly reported and investigated due lack of trained staff and scarce resources. The unit has partnered with the Pharmacy and Poisons (PPB) to have a robust and well-funded AEFI section.
Kenya is committed to the 1988 World Health Assembly resolution of global poliomyelitis eradication. Towards this end, the country has been implementing the four recommended strategies; Acute Flaccid Paralysis (AFP) surveillance, routine immunisation, National/Sub-national Immunisation Days and mop-up vaccination campaigns.
A lot of progress has been made in the performance of AFP and population immunity in the country since commencement of this initiative. The last indigenous wild poliovirus (WPV) in Kenya was in 1984.
However, the country suffered importations of WPV from Somalia and Sudan in 2006 (two cases in Garissa County) and 2009 (19 cases in Turkana County). One additional WPV type 1 case was detected in Kenya in July 2011 and was genetically linked to the 2010 outbreak in eastern Uganda (Bugiri district) and the 2009 outbreak in Kenya.
On 16th May 2013, a polio outbreak linked to the epidemic in Somalia was reported in Garissa County at a refugee camp. A total of 14 confirmed cases were reported by the time it was contained in July 2014.
Quarterly polio risk analysis is done based on the following:
- AFP surveillance performance indicators;
- Routine immunisation coverage; and,
- Surveillance index.
Based on these, gaps have been identified at sub-national level that require continuous support in terms of capacity building, support supervision, review meetings and conducting polio SIAs.
For measles, the current positivity rate is less than 10 percent and 40-5 percent for samples tested at Kemri’s EPI laboratory.
It is against this background that the country has decided to introduce rubella vaccine in the routine immunisation programme.
Despite the success achieved so far in measles case-based surveillance, there are challenges to the system. These are similar to those facing polio surveillance, but in addition, measles suffers a poor investigation rate by all counties due to lack of funds for shipment of specimens and inadequate capacity of health workers to conduct investigations due to high turnover of staff.
Kenya’s war on tuberculosis

The fight against TB in Kenya started soon after the Second World War but gained momentum after independence from Britain. The cumulative experience of dealing with TB over so many years has provided a sound basis for building a strong NTP and, in particular, for countering the impact of HIV, which dramatically increased the incidence of TB. Since 1990, the TB notification rate increased by a factor of six, mainly as a result of HIV.
Despite the increased burden of disease, the National Tuberculosis Control Programme (NTP) has been strengthened, cure rates have improved and rates of case detection have increased. Kenya has reached the 2005 targets for both case detection and cure.
There are now plans to continue improving the quality of programme data through the use of electronic reporting and recording systems, strengthen community involvement in TB control, engage all health service providers, strengthen TB control in congregate settings, re-examine the control of TB in nomadic areas, and to strengthen the control and treatment of drug-resistant TB.
In 2017, Kenya marked World Tuberculosis Day by releasing results of a study by the Ministry of Health (MoH) — the first of its kind since Kenya’s independence. It revealed that TB remains high in Kenya, and experts say the country still lags in the fight against the disease.
The survey represents a united front by many committed parties to determine the true burden of tuberculosis, and how to best combat the fourth-leading cause of death in Kenya.
The survey provided an accurate estimate of Kenya’s TB burden, revealed the challenges in delivering TB testing and treatment, and identified people with TB not yet detected by the NTP. It was conducted to inform the government on how to effectively respond to TB.
More than 63,000 people across 45 counties were screened for the survey and, for the first time, there was accurate data on TB’s prevalence. The report stated that there were more cases than previously estimated, with a TB prevalence of 558 per 100,000 people.
TB was found to be higher in men between the ages of 25 and 34 years, urban dwellers, and women over the age of 65.
The majority (83 percent) of TB cases were HIV negative, suggesting that broad efforts at controlling TB in people with and without HIV are needed.
Most people who exhibit TB symptoms such as dry cough usually buy medicine at local chemists. Early diagnosis is important in treating TB cases, though few chemists stock TB drugs because they are readily available in public and private health facilities.
The United States Agency for International Development (USAID) and the US Department of Health and Human Services’ Center for Disease Control and Prevention (CDC) provided technical and scientific support to the Government of Kenya in the design and implementation of the survey and $575,000 in funding to conduct it.
According to Kenya’s National Tuberculosis, Leprosy and Lung Disease Programme, the major factor responsible for the large TB burden is the concurrent HIV epidemic.
Other contributing factors include poverty and social deprivation that have led to a mushrooming of peri-urban slums between cities and the countryside, and limited access to general healthcare services.
The survey findings also reveal that the current practice of screening for TB symptoms and using microscopy as the only test misses many cases. Using GeneXpert, an innovative technology for diagnosis of TB, has led to the detection of 78 percent of TB cases among those screened.
The government has increased engagement with the private sector, and carries out targeted approaches through community-based action, and improved community awareness of TB symptoms to bring home the message that “TB can be treated”.
In March 2019, the MoH launched a new strategy to diagnose and cure at least 597,000 TB patients by the year 2023.
The National Strategic Plan for Tuberculosis, Leprosy and Lung Disease (2019-2023) was launched by then Cabinet Secretary Sicily Kariuki during the commemoration of the World Tuberculosis Day, at Thika Stadium, Kiambu County.
She said the strategy would ensure a patient-centered approach to TB prevention, diagnosis, treatment and care, that calls for elimination of fees associated with diagnostic testing, including chest radiography services.
“This is in line with President Uhuru Kenyatta’s commitment to have at least 597,000 people with TB treated by the year 2023, including 55,000 children, 542,000 adults and 4,500 people with Multiple Drug Resistant (MDR) TB, in addition to providing TB Preventive Therapy to at least 900,000 Kenyans at risk,” the CS said.
In addition, the CS launched the “Maliza TB County Initiative” to mobilise domestic efforts to support TB prevention, treatment and care. “This initiative will be piloted in Kiambu County. It is envisaged that by 2025, all the counties will be covered,” she said.
The CS urged all the partners to double their efforts towards finding all the missed cases and put them on treatment as per the national call: “Mulika TB, Maliza TB.”
In the past one year, Kenya reported and treated 96,434 TB patients, among them 10,087 children and 669 Multiple Drug Resistant (MDR) TB cases.
Though TB diagnosis, medicines and nutritional support are offered free in all government and faith-based health facilities, 40 percent of the cases are missed annually.
Currently, the Health Ministry is partnering with the Ministry of Education, Science and Technology in conducting school health programmes focusing on TB prevention.
“I would like to urge all other sectors, including line ministries and corporate entities, to identify and take up their crucial roles on TB response,” she said.
Tuberculosis (TB) remains a global threat to public health and is the leading cause of death by a single infectious agent, with 1.6 million deaths in 2017. An estimated 10 million people developed TB in 2017 but only 6.4 million (61%) were notified.
The global targets aim at 95 percent reduction in TB deaths, and 90 percent reduction in incidence compared to 2015 and 0 percent TB-affected families facing catastrophic costs due to TB by 2035 [2]. The true burden of TB needs to be ascertained so that efforts to find all incident cases are scaled up. In countries without high quality vital registration and health notification systems, TB prevalence surveys offer the best method of accurately measuring the TB burden.
Kenya is listed by the World Health Organisation (WHO) among the 30 high burden TB states. Despite the considerable investment done by the government and partners in TB care and prevention in the past 20 years, the disease is still the fourth leading cause of death.
The prevalence of bacteriologically confirmed pulmonary TB in those above 15 years in Kenya was found to be 558 (455–662) per 100,000 population. In Uganda, it was found to be 401 (292–509) per 100,000 adult population, Nigeria 524 (378–670) per 100,000 adult population, and Zambia 638 (502–774) per 100,000 adult population. In Tanzania, the prevalence was found to be 295 per 100,000 adult population, and in Ethiopia 277 (208–347) per100, 000 population.
Gender disparity in health seeking behaviour has been observed in HIV and TB care, showing a greater reluctance by men to seek healthcare when sick. In the survey, the confirmed cases, majority (65 percent) of those with symptoms who did not seek treatment were men.
This, together with the finding that men had a disproportionately high burden of TB – two and half times more than women and twice that reported through routine surveillance – shows that Kenya needs specific approaches to remove access barriers, reduce delays in diagnosis and improve management of TB.

In addition, the prevalence to notification gap was highest in the age group 25–34 and those over 65 years old. This indicates that there are many cases in these age groups who are not notified or not diagnosed. In the inventory study, under-reporting was found to be higher in those over 55 years old, which correlates with what was found in this survey. Operational research should be carried out to identify risk factors and understand why TB is being missed in these two age groups.
The percentage of individuals with TB symptoms who had not sought care was 67 percent in the survey. They may not have been experiencing severe symptoms yet, or they faced barriers to healthcare.
The TB patient study found that TB can impose profound costs on families, with a third of TB-affected households and two thirds of drug-resistant TB-affected households experiencing catastrophic health costs.
In addition, it highlighted that TB is a cause of poverty, with 28 percent of patients using negative coping mechanisms like taking loans, using savings and selling assets to meet medical expenses.
This means that people may not access healthcare due to financial difficulties. Addressing these financial barriers may encourage more people to seek treatment and help close the current case detection gap.
These findings call for sufficient investment in community TB health communication to increase awareness and encourage people to seek early intervention.
Health interventions in RMNCH in parts of Kenya have successfully invested in this approach by using school health programmes to target children as change agents within their families. In addition, strengthening systematic screening of selected high-risk groups, like all contacts of people with TB, can help identify patients with early symptoms.
Possible solutions lie in optimising TB surveillance to eliminate leakages, and developing and implementing approaches to systematically screen all people seeking care in health facilities.
